The management of melanoma has entered an era of biomarker-driven targeted therapy and immunotherapy. The following case, presented by Sanjiv S. Agarwala, MD, at PMO Live 2015, illustrates the 2015 approach to the management of metastatic melanoma.
Case: Metastatic Melanoma
A 56-year-old female with a history of T2N2b melanoma and no adjuvant therapy presents to the clinic with pain and fatigue. She was lost to follow-up after her primary diagnosis. A PET/CT scan shows multiple lung and liver metastases, and a biopsy confirms metastatic melanoma. An MRI showes no brain lesions. Her lactate dehydrogenase level is elevated at 420 IU/L, and ECOG performance status is 1. Genetic testing revealed a BRAF mutation.
Treatment Approach
What Would Be Your Approach?
- Chemotherapy
- Single-agent BRAF inhibitor
- Anti–CTLA-4 therapy with ipilimumab
- BRAF plus MEK inhibitor combination
- Single-agent anti–PD-1 therapy
- Combination anti–PD-1 and anti–CTLA-4 therapy.
“In the era of biomarker-driven targeted and immunotherapy, chemotherapy is obsolete as a frontline option for melanoma in the United States and in countries that have access,” said Dr Agarwala, Chief, Oncology and Hematology, St. Luke’s Cancer Center, Bethlehem, PA.
“What has changed in melanoma in the treatment paradigm is, you target something,” he said. Either the tumor can be targeted after discovering a driver mutation, or the host can be targeted with checkpoint inhibitors.
Anti–CTLA-4
CTLA-4 acts as a brake at the site of the T-cell; by taking the brake away with an anti–CTLA-4 agent, the T-cell becomes more powerful, he explained. The PD-1 pathway works not only on the T-cell side but on the tumor side as well, “and that is potentially why the PD-1 brake is probably a more important brake in terms
of immunotherapy.”
Anti–CTLA-4 therapy is superior to vaccines and chemotherapy: ipilimumab alone (N Engl J Med. 2010;363:711-723), or combined with chemotherapy (N Engl J Med. 2011;364:2517-2526), improved overall survival (OS) in naive and pretreated melanoma patients compared with dacarbazine.
Anti–PD-1 as Single Agent
Single-agent anti–PD-1 is effective for the treatment of melanoma in different settings and using different schedules. As monotherapy, anti–PD-1 therapy with pembrolizumab was also superior to anti–CTLA-4 therapy with ipilimumab on the end point of OS in patients with advanced melanoma in the KEYNOTE-006 trial (AACR 2015. Abstract CT101). The results from this study support pembrolizumab as a frontline option for this indication when immunotherapy is chosen.
Anti–CTLA-4 and Anti–PD-1 Together
Anti–CTLA-4 and anti–PD-1 therapy in combination was superior to either therapy alone in the CA209-67 trial, in which nivolumab plus ipilimumab extended median progression-free survival to 11.5 months, compared with 6.9 months for nivolumab alone and 2.9 months for ipilimumab alone (ASCO 2015. Abstract LBA1). Grade 3/4 toxicity, however, was greater in the combination group compared with the 2 monotherapies. “Most of us think we should wait for overall survival” before definitively declaring the combination to be superior.
An immunotherapy biomarker to guide treatment is desired; preliminary data indicate that combination immunotherapy may be advantageous over monotherapy if PD-L1 expression is <5% (ASCO 2015. Abstract LBA1).
BRAF inhibition: Alone or in Combination
with a MEK Inhibitor
About 50% of melanomas have an activating BRAF mutation. The BRAF inhibitor vemurafenib was associated with a significantly higher rate of confirmed response and an improved OS compared with dacarbazine in patients with previously untreated stage IV BRAF V600–mutant melanoma (N Engl J Med. 2011;364:2507-2516). More recently, the combination of dabrafenib and the MEK inhibitor trametinib improved 2-year median OS compared with dabrafenib alone (25.1 vs 18.7 months; hazard ratio, 0.71; P = .011) (Lancet. Published online May 29, 2015). Interestingly, toxicity was less with the combination than with monotherapy.
“The BRAF inhibitors work very quickly, within 24 to 48 hours, but they don’t last very long” said Dr Agarwala. “Immunotherapy needs some time, especially anti–CTLA-4, which needs about 3 months to work. Anti–PD-1 is quicker; maybe 4 to 6 weeks. The combination…may be even faster than that, but in general, immunotherapy has a delayed start but a longer duration.”
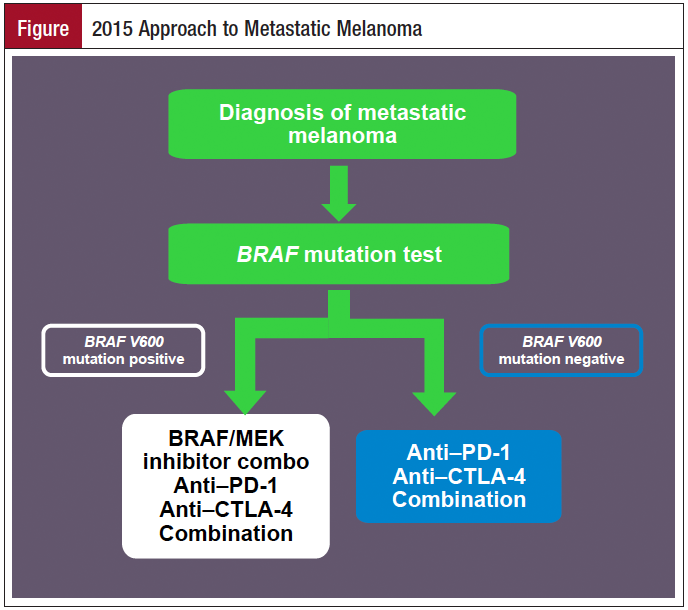
Algorithm in 2015
A treatment algorithm in 2015 for metastatic melanoma starts with a test for BRAF mutations. If the patient tests negative for BRAF V600 mutations, a BRAF inhibitor is not indicated. With a BRAF V600 mutation, combination BRAF/MEK inhibitor and immunotherapy with either an anti–PD-1 or anti–CTLA-4 agent, or their combination, are frontline choices.