Genetic tumor profiling, immune profiling, and immunohistocompatibility expression profiling are performed routinely at Yale Cancer Center for patients diagnosed with cancer. The results are presented to the multidisciplinary Molecular Tumor Board, which meets weekly to make treatment decisions. The following case exemplifies a personalized medicine approach and was presented by Roy S. Herbst, MD, PhD, at the Third Annual PMO Live conference.
Case: Non–Small Cell Lung Cancer
A 77-year-old former smoker (25-pack-year history) presented for a second opinion regarding newly diagnosed non–small cell lung cancer. The patient had noticed increased dyspnea on exertion over past year, and cough with sputum production.
A chest radiograph showed a left upper lobe (LUL) mass. Computed tomography showed a 25×14-mm irregular LUL paramediastinal parenchymal lesion abutting the pleura. Pulmonary function tests revealed normal lung function. Brain magnetic resonance images were negative. LUL core biopsy revealed well-differentiated adenocarcinoma of the lung.
The patient underwent robotic lobectomy with lymph node dissection. Pathology revealed a 4-cm moderately to well-differentiated adenocarcinoma of the lung with 50% papillary, 30% acinar, and 20% micropapillary histology. Bronchial and vascular margins were negative. The patient had evidence of visceral pleural invasion. One lymph node, L12, was positive for carcinoma; the others were negative.
Would You Recommend Tumor Genetic Profiling?
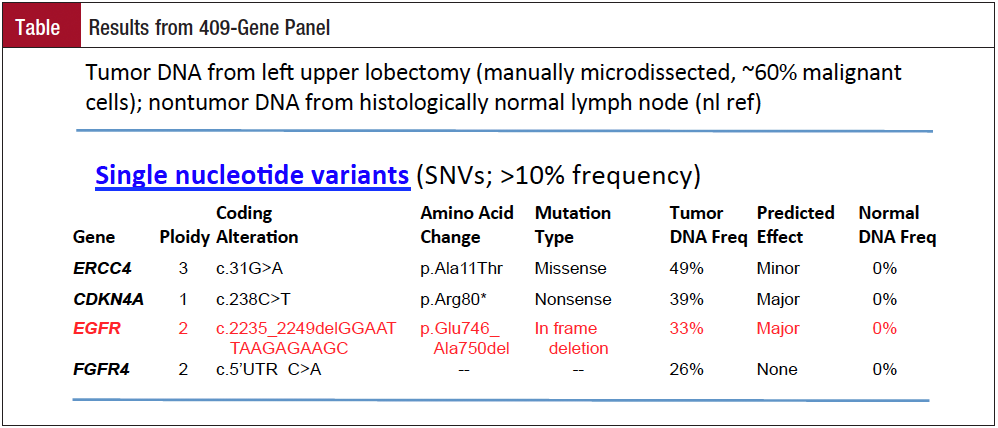
Tumor tissue was tested in a 409-gene panel. “You would at least need to know ALK fusion and EGFR mutation status,” said Herbst, Chief of Medical Oncology, Yale Cancer Center and Smilow Cancer Hospital at Yale-New Haven, CT.
Single nucleotide variants with >10% frequency were present at ERCC4, CDKN4A, EGFR, and FGFR4 (Table). “The one that stands out is an EGFR in-frame deletion in exon 19, which is quite common,” he said. Thirty-three percent of the tumor DNA had this mutation.
How Would You Treat the Patient?
Mutations in exons 19 and 21 are known to have response rates to an EGFR tyrosine kinase inhibitor (TKI) of as high as 80%. These mutations are most common in never-smokers, females, patients with East Asian ethnicity, and adenocarcinomas.
The patient felt well overall after surgery. Adjuvant chemotherapy was recommended before the results from sequencing were known. The Molecular Tumor Board recommended chemotherapy and suggested consideration of an EGFR TKI on progression. Approved and investigational agents for this mutation are first-generation reversible TKIs (gefitinib, erlotinib), the second-generation irreversible TKI afatinib, and third-generation mutation-specific TKIs (CO-1686, AZD9291).

